Opioid use disorders have become increasingly common in recent years, often with devastating consequences. Opioid-related overdose deaths have skyrocketed, and illegal use of the opioid heroin has seen a major resurgence.
Opioid addiction can be very challenging to overcome, especially for people who try to quit without professional help. Opioids have a profound effect on brain chemistry, and changes can persist for months or even years after someone has quit taking opioids.
The Opioid Crisis
In the U.S., chronic pain is one of the most common reasons why people see their doctors. Opioids like morphine have long been used as powerful pain-killers, but morphine is also notoriously addictive. Consequently, doctors are hesitant to write prescriptions for morphine. As new semi-synthetic and synthetic opioids were developed and marketed, pharmaceutical companies emphasized that their opioids were not addictive. This gave medical care providers a new way to help people manage chronic pain. Unfortunately, the new generation of opioids is at least as addictive as morphine, and more than two million Americans are currently struggling with an opioid use disorder.
What are Opioids?
Opioids are a large class of drugs that are used medicinally and recreationally. Morphine was one of the earliest types of opioid that was widely used, and since the discovery of morphine, several other types of opioids have been created. Opioids exert their effects by hijacking normal brain signaling pathways that regulate pain and pleasure. This is why opioids are so good at killing pain, and it’s also why they are so addictive. When people abuse opioids recreationally, they experience intense euphoria that reinforces addiction.
Recovery Can Be Life Changing
Whether you or a loved one is struggling with addiction, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
“My life has became something that I’m proud of and something I can be grateful for.“
– Joseph McDermott, The Recovery Village Cherry Hill Alumni
Signs & Symptoms of Opioid Use
Opioid use disorders are usually associated with some hallmark signs and symptoms that can help identify whether you or someone you love is at risk.
Physical signs of opioid use:
- Drowsiness
- Confusion
- Muscle flaccidity
- Cold, clammy skin
- Poor motor coordination
- Constricted pupils
- Shallow breathing
- Slow heart rate
- Stupor or unconsciousness
Psychological symptoms of opioid use:
- Euphoria
- Reduced libido
- Lethargy
- Rapid mood swings
- Confusion
Physical symptoms of opioid use:
- Dry mouth
- Constipation
- Dizziness
- Muscle weakness
- Lack of coordination
- Sleeping too much
- Nausea
Behavioral signs of an addiction:
- Preoccupation with getting and using opioids
- Missing work or school
- Evasiveness or unusual secrecy
- Inability to concentrate
- Failure to meet normal responsibilities
- Loss of interest in friends or hobbies
- Inability to quit taking opioids or reduce the dose
In addition, people with opioid use disorders often face social consequences, including: financial troubles, legal troubles and job loss.
Side Effects of Opioid Use
Side effects are unintended consequences that occur when you take a drug. Opioid use disorders have been linked to serious side effects, some of which can have long-term health consequences. Side effects may include:
- Altered immune system function
- Hormonal changes
- Increased sensitivity to pain
- Sleep disturbances
- Reduced motor coordination
- Bladder dysfunction
Withdrawal & Detox Process
Different types of opioids are associated with somewhat different withdrawal and detox processes, but several generalizations can be made. The opioids that are associated with the most challenging withdrawal process are highly potent opioids with short half-lives (e.g. fentanyl, heroin, oxycodone). When someone uses these drugs, they experience a rapid high that is short-lived, which increases the risk of developing an addiction.
Opioid withdrawal is generally not associated with significant health risks, but withdrawal symptoms can be profoundly uncomfortable and debilitating. The risk for relapse is high in the first days and weeks of recovery, especially among people who quit cold turkey and without professional help. Anyone who wants to quit taking opioids should make an appointment with an addiction specialist who is experienced with opioid withdrawal and recovery.
Withdrawal Timeline
Opioids are a large class of drugs, so withdrawal timelines vary somewhat depending on the specific opioid. Drugs that are metabolized quickly have a faster onset of withdrawal symptoms, but the duration is shorter than drugs that take longer to metabolize. Other factors that can influence the withdrawal timeline include the degree of dependence, age, and metabolism.
Oxycodone and heroin are among the most common opioids of abuse, and they have similar withdrawal timelines. Approximately 8-12 hours after the last dose is taken, withdrawal symptoms will begin to set in. Symptom severity peaks between 36-72 hours after the last dose, and withdrawal ends within 7-10 days.
Withdrawal Symptoms
Most people will experience withdrawal symptoms within a few hours of their last dose. This is the detoxification and acute withdrawal period, during which time all of the opioids in your system are metabolized.
Physical symptoms of opioid withdrawal:
- Runny nose
- Watery eyes
- Frequent yawning
- Sweating and/or chills
- Nausea/vomiting
- Diarrhea
- Muscle cramps
- Insomnia
Psychological symptoms of opioid withdrawal:
- Dysphoria (a general sense of unease or dissatisfaction)
- Anhedonia (inability to experience pleasure)
- Depression
- Anxiety
- Cravings
- Restlessness
- Irritability
- Mood swings
Read more: How Long Do Opioids Stay in Your System?
Medication-Assisted Treatment
Medical detox and medication-assisted treatment (MAT) are not the same. The goal of medical detox is to successfully get someone through the initial period of detoxification and withdrawal, and medications like benzodiazepines might be provided if symptoms are severe. The goal of MAT is to help people manage long-term withdrawal symptoms that can persist for months or even years after someone quit taking opioids. MAT drugs are long-acting opioids that do not cause the euphoric high that opioids of abuse are known for. MAT drugs have similar chemical effects in the brain (thus preventing withdrawal), but they do not reinforce addiction.
Common MAT Drugs
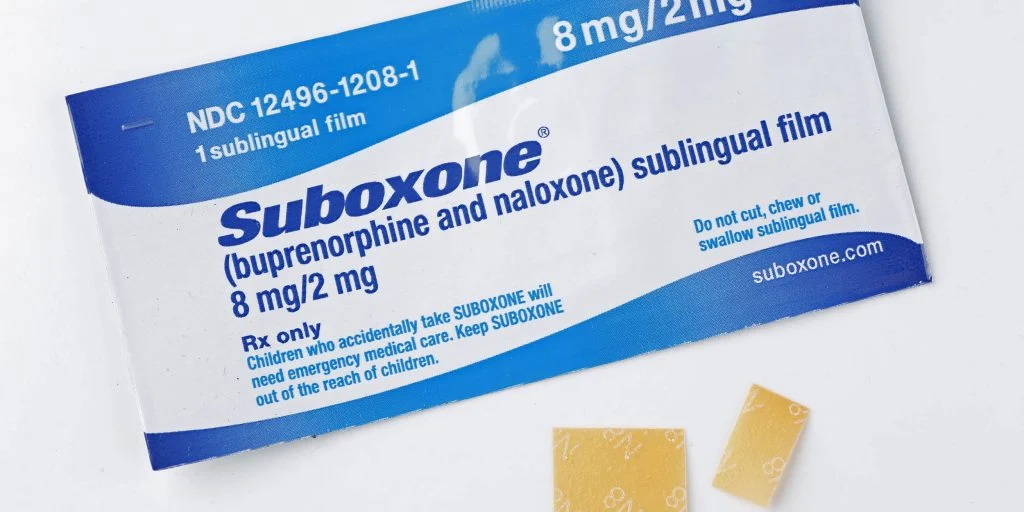
Buprenorphine and methadone are both known as “opioid agonists,” meaning that they activate opioid receptors in the brain. When they are taken as prescribed, they are not associated with a risk for abuse. However, high doses can get people high, so there is some risk for abuse.
Naloxone is an “opioid antagonist,” meaning that it actually blocks opioid receptors from interacting with opioids. When buprenorphine/naloxone is taken as prescribed, the naloxone is inactive and buprenorphine can prevent withdrawal symptoms from setting in. However, if buprenorphine/naloxone is injected into the bloodstream, the naloxone is activated and prevents buprenorphine from interacting with opioid receptors.
Opioid Addiction Treatment Options
Anyone who wants to quit taking opioids is urged to make an appointment with an addiction specialist who can provide recommendations and referrals. Opioids are notoriously challenging to quit, and working with a rehab professional is the best way to successfully overcome an opioid use disorder.
The Recovery Village Cherry Hill offers a range of opioid addiction treatment options:
- Medical Detox: Medical detox is often the first step in opioid recovery. People in medical detox are supervised around-the-clock by medical professionals. When appropriate, medications that can ease withdrawal symptom severity can be provided.
- Residential Rehab: Relapse rates in the first few weeks of recovery are high. Residential (or inpatient) rehab programs give clients a safe environment that protects them from triggers and temptation.
- Outpatient Rehab: Many people with opioid use disorders transition from residential programs to outpatient care. Outpatient programs vary from all-day/every-day programs to weekly or bi-weekly therapy sessions.
- Aftercare: Once rehab is over, many people continue to participate in aftercare programs. Aftercare can be a valuable way for people in recovery to meet like-minded people and participate in drug-free activities.
- Co-Occurring Disorders: Mental health disorders are often overlooked in opioid use disorders. Quality treatment programs will evaluate their clients for co-occurring disorders and tailor their treatment plan to address both the mental health and opioid use disorders.
Related Topic: Inpatient vs. Outpatient Rehab
FAQs
Some frequently asked questions about opioids are addressed below.
What’s the difference between opiates and opioids?
“Opiate” and “opioid” are often used interchangeably, but there is a difference. Opiates are generally considered to be naturally produced by the opium poppy. Opiates include morphine and codeine. Opioids can be semi-synthetic, meaning they are modified versions of natural opiates, or synthetic, meaning they are completely man-made. Semi-synthetic opioids include oxycodone and heroin. Fentanyl is the most common synthetic opioid.
Why are opioids so addictive?
Our brains have an “endogenous opioid system” that helps regulate pain and pleasure. Normally, endogenous (naturally produced) opioids and dopamine work together to tell the brain when something positive happens. For example, eating chocolate causes endogenous opioids and dopamine to be released, which teaches the brain that chocolate is good. Opioids of abuse hijack this system and cause huge amounts of dopamine to be released. The brain interprets this surge of dopamine to mean that something really great happened, so the brain incorrectly links opioid use to positive outcomes. Regular opioid abuse causes physical and chemical changes in the brain that strongly reinforce dependence and addiction.
Which opiates are the most addictive? Are all opioids addictive?
The most addictive opioids are the ones that have the strongest effects on the brain. Synthetic opioids like fentanyl and its derivatives are far stronger and more addictive than nearly any other addictive drug, including heroin. Fentanyl is commonly prescribed to treat severe pain or as an anesthetic agent during surgery. Unfortunately, fentanyl is easy to make in a lab, and there are hundreds of derivatives that are astonishingly potent. Carfentanil is a fentanyl derivative that is 10,000 times more potent than morphine, and it is currently used as an elephant tranquilizer by veterinarians. There is no approved use for carfentanil in humans, but it is being found in confiscated drugs and in people who died from opioid-related overdoses.
What drugs are considered opioids?
The opioid class of drugs is quite large and includes endogenous opioids (opioids that we make in our bodies), naturally produced opioids, semi-synthetic opioids, and fully synthetic opioids.
Examples of common opioids of abuse include:
- Heroin
- Morphine
- Codeine
- Oxycodone
- Hydrocodone
- Fentanyl
- Carfentanil
What contributed to the opioid crisis?
There are several factors that contributed to the development of the opioid crisis, but many experts point to profit-motivated pharmaceutical companies as the most important driver of the epidemic. The brand name drug OxyContin was approved by the U.S. Food and Drug Administration (FDA) in 1995. Between 1999 and 2017, deaths related to prescription opioids increased by about 430%. While this does not directly implicate pharmaceutical companies, other data do. For example, one study found that opioid overdose deaths increase in areas where pharmaceutical companies spend money to market their drugs. In recent years, federal charges have been levied against some of the biggest pushers of prescription opioids.
From 1999 to 2010, the rate of opioid addiction treatment increased by about 600%, raising concerns about the addictive nature of prescription opioids. Between 2010-2012, new laws and regulations were enacted to reduce the availability of prescription opioids. An unforeseen consequence of this crackdown was that people with opioid use disorders turned to heroin. Heroin use in America had been relatively stable for decades, but a substantial increase in heroin overdose deaths was observed in 2011, and heroin overdose deaths increased by more than 400% between 2010 and 2017.